- Our Doctors
- Our Specialities
Super Speciality
-
 Advanced Diagnostic and Interventional Radiology
Advanced Diagnostic and Interventional Radiology -
 Anesthesiology & Pain Management
Anesthesiology & Pain Management -
 Clinical Nutrition and Dietetics
Clinical Nutrition and Dietetics -
 Critical Care
Critical Care -
 Dental and Maxillofacial Surgery
Dental and Maxillofacial Surgery -
 Dermatology
Dermatology -
 Emergency and Trauma
Emergency and Trauma -
 Endocrinology and Metabolic Disease
Endocrinology and Metabolic Disease -
 Family Medicine
Family Medicine -
 General and Laparoscopic Surgery
General and Laparoscopic Surgery -
 General Medicine
General Medicine -
 GI Surgery, Advanced Laparoscopy and Gastro Oncosurgery
GI Surgery, Advanced Laparoscopy and Gastro Oncosurgery -
 Head and Neck Oncology
Head and Neck Oncology -
 Heart and Lung Transplant
Heart and Lung Transplant
-
- Key Procedures
- Our Hospitals
- International Patient
- Contact us
-
Quick Links











Conditions and Treatments
Uncompromised healthcare services. Always.
- Our Specialties
- Treatments
- Diseases
Meet Our Doctors
Experienced medical professionals for a superior patient experience.
Dr. George Abraham
Chair & Senior Consul...
Centre for bone, joint & spine
View Profile Book an AppointmentDr. Murali P Vettath
Chair & Senior Consul...
Centre for heart & vascular ca...
View Profile Book an AppointmentDr. Shafeeq Mattummal
Chair & Senior Consul...
Centre for heart & vascular ca...
View Profile Book an AppointmentDr. Anil Saleem
HOD & Senior Consulta...
Centre for heart & vascular ca...
View Profile Book an AppointmentDr. Sachin Sureshbabu
HOD & Senior Consulta...
Centre for neurosciences
View Profile Book an AppointmentDr. Geetha George
HOD & Senior Consulta...
Anesthesiology & pain manageme...
View Profile Book an AppointmentDr. Anudath Brahmadat...
HOD & Senior Consulta...
Centre for neurosciences
View Profile Book an AppointmentDr. Sameer Ali Parava...
HOD & Senior Consulta...
Centre for bone, joint & spine
View Profile Book an Appointment+
Doctors
+
Locations
+
Lives Healed
+
Beds
Our Hospital Networks
Meitra works closely with its partners to reduce disparities in healthcare, improve access and increase vital resources for those in need. We seek to leverage our expertise in prevention, patient care, and education to make the greatest impact in the community.
Find Hospital Near YouHear It From Our Patient
Real people, real stories. Our patients share their experiences of their recovery journey.
Bilateral TKR / Dr.Sameer Ali - Meitra Hospital
Treated by : Dr. Sameer Ali Paravath
Patient's Successful Partial Knee Replacement Story
Treated by : Dr. Sameer Ali Paravath
Spine Surgery Patient Testimonial
Treated By: Dr Vinod
Sri Lankan Native Returns Home in Just a Week, After a Successful TAVR Procedure
Treated by: Dr Ali Faizal and Dr Asish Kumar Mandalay
Successful Transcatheter Aortic Valve Replacement procedure | Meitra Hospital, Calicut
Treated By: Dr. Ali Faizal and Dr. Asishkumar Mandalay
Successful TAVR Procedure Avoid Leg Amputation through Balloon Angioplasty | Meitra Hospital
Treated by: Dr Ashishkumar Mandalay
Meitra United Heart Centre: Comprehensive Cardiac Care in Kasaragod
News and Social Update
Stay updated on the recent events and health check-up programs at our hospital.
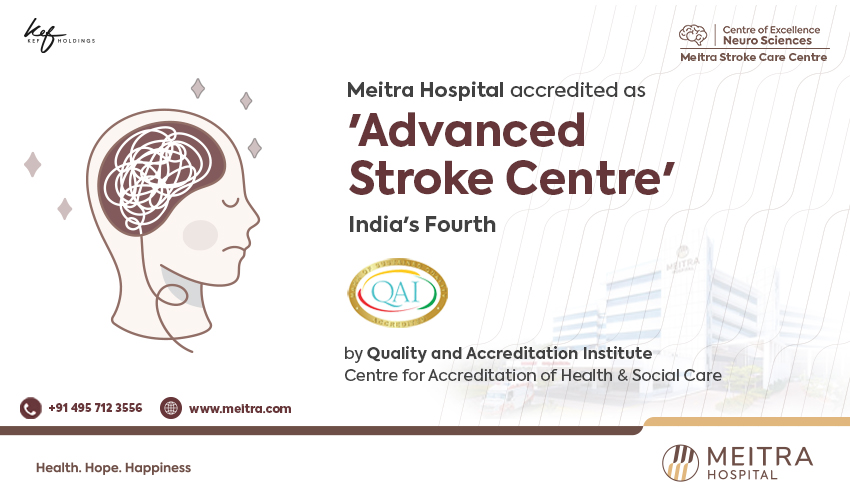
സ്ട്രോക്ക് അറിയേണ്ടതെല്ലാം | Stroke - Symptoms and causes | Meitra Hospital Calicut
സ്ട്രോക്ക് അറിയേണ്ടതെല്ലാം | Stroke - Symptoms and causes | Meitra Hospital Calicut A stroke, sometimes called a brain attack, occurs when something blocks blood supply to part of the brain or when a blood vessel in the brain bursts. In either case, parts of the brain become damaged or die. A stroke can cause lasting brain damage, long-term disability, or even death.
Doctors Talk
Gall Bladder Stones | പിത്താശയക്കല്ലുകള് ഒഴിവാക്കാം | Dr Shanavas Kakkat | Meitra Hospital Calicut
Dr.Shanavas Kakkat, Consultant - GI Surgery , Centre of Excellence for Gastro Sciences, is explaining about the symptoms and treatment of Gall bladder stones. Gallstones are hardened deposits of digestive fluid that can form in your gallbladder. Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, just beneath your liver. The gallbladder holds a digestive fluid called bile that's released into your small intestine.

 +91 9393 108 108
+91 9393 108 108